Our earlier epidemiology study linked cannabis use to cardiovascular disease in people. Because most people smoked cannabis in US population at the time, we could not distinguish the effects of inhaled cannabis from other forms of consumption, particularly edibles. Leila Mohammadi and her UCSF colleagues new paper “Association of Endothelial Dysfunction With Chronic Marijuana Smoking and THC-Edible Use” shows that both smoked cannabis and edibles adversely affect blood vessel function which predicts later heart disease and heart attacks.
They recruited people who did not use tobacco in to 3 groups: marijuana smokers (=3 smoking sessions per week for at least 1 year), tetrahydrocannabinol (THC)–edible users (=3 edibles per week for at least one 1 year), and cannabis nonusers. They then measured the ability of their arteries to expand in response to increased demand for blood flow using flow mediated dilation. FMD is measured by temporarily blocking blood flow using a blood pressure cuff, then measuring how much larger arteries become when the cuff is released, allowing a rush of blood to service the oxygen-starved arm tissue below the cuff.
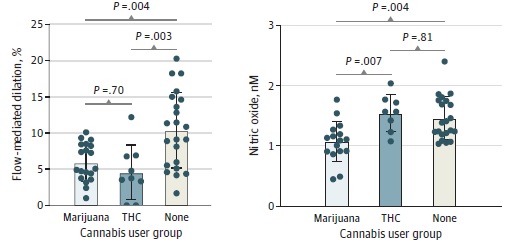
They found FMD cut by about half, from the arteries’ diameter increasing by about 10% in people who did not use cannabis to about 5% in both people who smoked marijuana (“marijuana’ in left graph above) and consumed edibles (“THC”). These effects are comparable to the effects of tobacco smoking.
It is well-established that smoking both marijuana and tobacco depresses FMD by reducing arteries’ production of nitric oxide, which dilates the arteries. Consistent with this earlier work, nitric oxide production was cut in marijuana smokers (right graph above) compared to nonusers. In contrast, nitric oxide production was not significantly different in people who consumed edibles compared to nonusers. Thus, even though consuming edibles had similar adverse effects on arterial function as smoking, edibles are not acting by depressing nitric oxide production. In other words, marijuana smoking and edible consumption were both associated with similar adverse effects on arterial function similar to that observed in tobacco smokers, but through different mechanisms.
In addition, there are dose-response relationships, with bigger reductions in FMD among people who smoked or ate more cannabis per week.
This paper not only adds to our general understanding of how cannabis consumption adversely affects the cardiovascular system, but provides important new evidence that edibles as well as smoked cannabis adversely affects he cardiovascular system.
Here is the abstract:
Importance: Recreational and medicinal cannabis legalization has led to increased cannabis use. To understand the consequences for vascular health, we initiated the CANnabis: Does It Damage Endothelium (CANDIDE) study.
Objective: To investigate whether cannabis use is associated with vascular endothelial dysfunction.
Design, setting, and participants: In this cross-sectional study, sex- and age- matched healthy adults, aged 18 to 50 years, living in the San Francisco Bay Area, California, who neither smoke tobacco nor vape and were not frequently exposed to secondhand smoke were recruited into 3 cohorts: 2 chronic cannabis user groups (marijuana smokers and tetrahydrocannabinol [THC]-edible users) and 1 nonuser group. Participants were recruited from October 25, 2021, through August 1, 2024; analysis was completed September 2024. Participants’ arterial flow-mediated dilation (FMD) and carotid-femoral pulse wave velocity (PWV) were measured. Human umbilical vein endothelial cells (HUVECs) were exposed to participant sera with and without vascular endothelial growth factor (VEGF) to assess the effects of user serum on endothelial nitric oxide production.
Main outcomes and measures: FMD and PWV were direct physiological measurements, and VEGF-stimulated nitric oxide production was measured from HUVECs incubated in user serum samples.
Results: Among 55 participants (20 female [37%]; 35 male [63%], mean age, 31.3 [SD, 8.4] years) arterial FMD was significantly lower among the marijuana smokers (mean, 6.0% [SD, 2.6%]; P = .004) and lower among THC-edible users (mean, 4.6% [SD, 3.7%]; P = .003) than among nonusers (mean, 10.4% [SD, 5.2%]). VEGF-stimulated nitric oxide levels in endothelial cells treated with participants’ sera were significantly lower for the marijuana smoker group (mean, 1.1 nmol/L [SD, 0.3 nmol/L] ) than for the nonuser group (mean, 1.5 nmol/L [SD, 0.3 nmol/L]; P = .004) but were unaffected among the THC-edible users group compared with the nonusers (mean, 1.5 nmol/L [SD, 0.3 nmol/L]; P = .81). FMD was inversely correlated with smoking frequency (r = -0.7; P < .001) and the amount of THC ingested (r = -0.7; P = .03). Other vascular properties showed no differences.
Conclusions: This cross-sectional study found that chronic cannabis smoking and THC ingestion were associated with endothelial dysfunction similar to that observed in tobacco smokers, although apparently occurring via distinct mechanisms.
The full citation is: Mohammadi L, Navabzadeh M, Jiménez-Téllez N, Han DD, Reagan E, Naughton J, Zhou LY, Almeida R, Castaneda LM, Abdelaal SA, Park KS, Uyemura K, Cheung CP, Onder MN, Goyal N, Rao P, Hellman J, Cheng J, Wu JC, Marcus GM, Springer ML. Association of Endothelial Dysfunction With Chronic Marijuana Smoking and THC-Edible Use. JAMA Cardiol. 2025 May 28. doi: 10.1001/jamacardio.2025.1399. Epub ahead of print. PMID: 40434782.It is available here.
Press coverage