Karin Kasza and colleagues new well-done study, “Divergence in Cigarette Discontinuation Rates by Use of Electronic Nicotine Delivery Systems (ENDS): Longitudinal Findings From the United States PATH Study Waves 1-6,” uses the large national PATH study to see if there were differences in real-world trends of adults stopping smoking before and after fourth generation e-cigarettes (pioneered by Juul) appeared. Fourth generation e-cigarettes add acid to the e-liquid, which generates nicotine salts that are easier to inhale, increasing the effective nicotine dose. Kasza and colleagues hypothesized that these new e-cigarettes would be associated with more smokers stopping smoking that older e-cigarettes that did not deliver nicotine as well.
That’s exactly what they found.
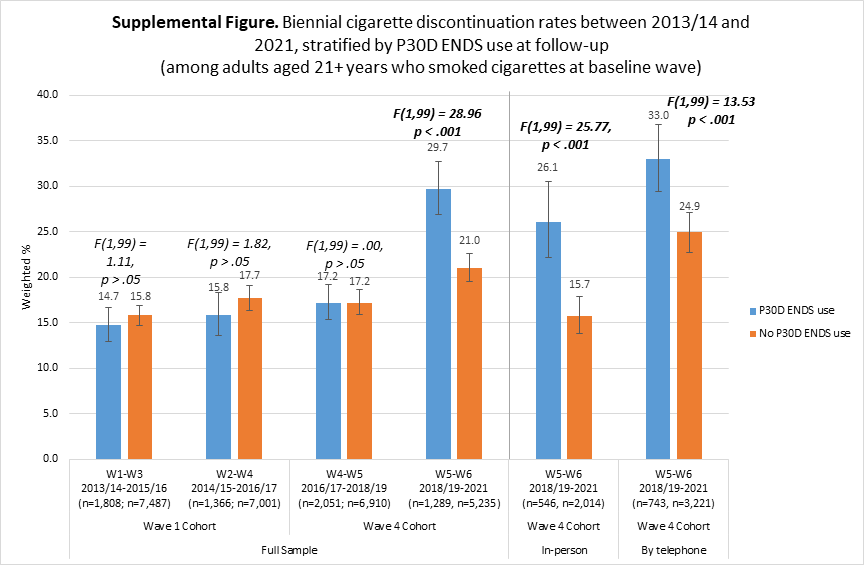
Between 2013/14 and 2015/16 e-cigarette use by smokers was not associated with stopping smoking: about 16% of smokers who did and did not use e-cigarettes stopped smoking cigarettes. This finding is consistent with our and others’ meta-analyses finding no association between e-cigarette use and stopping smoking in the real world during the same time period.
In contrast, between 2018/19 and 2021, about 30% of smokers who also used e-cigarettes (dual users) stopped smoking cigarettes compared to 20% of smokers who did not use e-cigarettes . (Compare first three pairs of columns with the fourth pair in the figure below.) Kasza and colleagues reached this conclusion by separating smokers based on their e-cigarette use at the beginning of each two-year period with having stopped cigarette smoking at the end. This longitudinal design where the exposure (e-cigarette use) precedes the outcome (having stopped smoking cigarettes) is the strongest kind of epidemiological study.

But, is this really good for health?
This increased stopping smoking among e-cigarette users seems like a good thing, but these people (30% of smokers) continued their nicotine addiction using e-cigarettes. The figure below shows the association between having stopped smoking and e-cigarette use at the end of the two years. (This cross-sectional association is virtually identical to the longitudinal results in the primary analysis above.) Note that the percentage of smokers who were continuing to use e-cigarettes at the end of the study (29.7% for the 2018/19-2021 period) is virtually the same (30.9%) as were using e-cigarettes at the beginning.
The assumption has been that, because they don’t burn tobacco, e-cigarettes are substantially safer than cigarettes, so these now-former smokers are better off, despite the fact that they are now addicted to nicotine delivered by e-cigarettes.
But the reality, based on 107 large population studies of the association between e-cigarette use and actual disease, is quite different. In particular, these 30% of smokers will continue to suffer the ongoing risks of e-cigarette use which have similar risks to cigarettes for some diseases and nearly as high a risk for others (open access link to meta-analysis). In addition, before they stopped smoking, they were dual users of both cigarettes and e-cigarettes, which is more dangerous than just smoking.
In contrast, the 20% of smokers who stopped smoking without using e-cigarettes are now nicotine-free and achieve rapid reductions in disease risk.
Kasza and colleagues’ result is broadly consistent with a meta-analysis of randomized controlled trials of e-cigarettes that found that smokers assigned to e-cigarettes were about half as likely (OR 0.50; 95% CI 0.32-0.77) to be nicotine-free at the end of the trial than those randomized to NRT.
Thus, accounting for the ongoing risks of e-cigarette use, a likely implication of this paper is that, despite being associated with more stopping smoking, the presence of fourth generation e-cigarettes is increasing harm by simply shifting people to being addicted to e-cigarettes, with all the attendant health risks.
And, of course, the ongoing harm to adult users does not consider adverse effects of fourth generation e-cigarettes like Juul on addicting kids who had never smoked before, something FDA also needs to consider when deciding whether these fourth generation e-cigarettes are “appropriate for the protection of public health.”
Here is the abstract:
Introduction: We compare real-world trends in population-level cigarette discontinuation rates among adults (ages ≥21) who smoked cigarettes, by electronic nicotine delivery systems (ENDS) use.
Aims and methods: U.S nationally representative data from adults in the Population Assessment of Tobacco and Health (PATH) Study (2013/14-2021, Waves 1-6) who smoked cigarettes in the past 30 days (P30D) were analyzed (n = 13 640). The exposure was P30D ENDS use. The outcome was P30D cigarette discontinuation at biennial follow-up. Weighted trend analyses were conducted to test for differences in cigarette discontinuation trends by ENDS use.
Results: Between 2013/14 and 2015/16, cigarette discontinuation rates were both 16% for those who used ENDS and for those who did not; between 2018/19 and 2021, rates were ~30% for those who used ENDS and ~20% for those who did not; the time by ENDS use interaction was significant.
Conclusions: The relationship between adults’ ENDS use and cigarette discontinuation in the context of an expanded ENDS marketplace, new tobacco regulatory actions, and COVID-19 differs from the relationship in earlier years.
Implications: It is important for public health decisions to be informed by research based on the contemporary ENDS marketplace and circumstances.
The full citation is: Kasza KA, Tang Z, Seo YS, Benson AF, Creamer MR, Edwards KC, Everard C, Chang JT, Cheng YC, Das B, Oniyide O, Tashakkori NA, Weidner AS, Xiao H, Stanton C, Kimmel HL, Compton W, Hyland A. Divergence in Cigarette Discontinuation Rates by Use of Electronic Nicotine Delivery Systems (ENDS): Longitudinal Findings From the United States PATH Study Waves 1-6. Nicotine Tob Res. 2024 Apr 3:ntae027. doi: 10.1093/ntr/ntae027. Epub ahead of print. PMID: 38566367. It is available here.

Why it’s almost as if e-cigs were never designed to be a health product.
Imagine a product that fails 3 out of 4 people who use it. And it has serious health risks: heart disease, lung disease. And the 1 in 4 it works for, are generally exposed to its risks indefinitely. Now imagine we’re just now finding that out, after millions have been sold, because the manufacturer did no testing for any of this. Does that sound like it was designed to be a health product?
LikeLike